Spectrum of placental changes in Pregnancy Induced Hypertension
Keywords:
Placenta, Pregnancy Induced Hypertension (PIH), Villous Abnormalities
Abstract
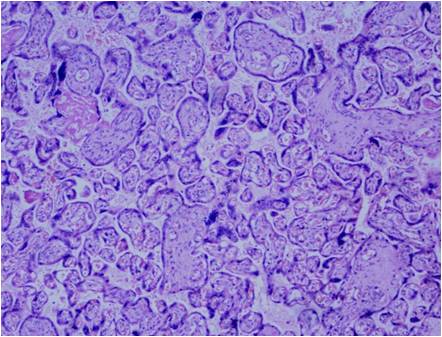
Background - PIH also known as toxaemia of pregnancy, is a major cause of maternal and perinatal morbidity and mortality worldwide. The present study was hence undertaken to analyse the effects of PIH on placenta as these changes serve as a guide to the duration and severity of disease.Methods - A prospective hospital based study was conducted from July 2012 to July 2013 in Department of Pathology, J.L.N. Medical College, Ajmer (Rajasthan). The study was done in 60 placentae, 30 placentae from uncomplicated full term deliveries formed the “Control Group” and 30 placentae from hypertensive pregnancies formed the “Study Group”. Sections were taken from placenta and processed for histopathological examination.Results - The striking villous abnormalities observed in the study group were cytotrophoblastic proliferation (83.34%), thickening of basement membrane (66.67%), fibrinoid necrosis (36.67%), obliterative endarteritis (60%), decreased villous vascularity (60%) and paucity of vasculosyntitial membranes.Conclusion - The gross abnormalities and villous lesions in PIH (p<0.001) were statistically significant. DOI: 10.21276/apalm.2017.1115References
1. Benirshkek. Pathology of the human placenta 2nd ed. New York: Springer Verlog;1990.
2. Jain K, Kavi V, Raghuveer C et al . Placental Pathology in PIH with or without IUGR. Indian J. Pathol. Microbiol.2007; 50 (3) : 533-537.
3. Emin M, Anna I. Bakardjiev, Susan J. The placenta : transcriptional, epigenetic, and physiological integration during development. J Clin Invest. 2010; 120(4) : 1016–25.
4. Udainia A, Jain ML. Morphological study of placenta in pregnancy induced hypertension with its clinical relevance, J Anat Soc. India. 2001; 50(1): 24-27.
5. Fernando Arias. In: Mosby. Practical guide to high-risk pregnancy and delivery. 2nd Edition. Harcourt Asia Private Ltd; 2000:184-185.
6. Cunningham F, Leveno K, Bloom S, Hanth J, Rouse D, Spong C. Pregnancy hypertension. In: Williams Obstetrics. 23rd ed. New York : McGraw Hill ; 2009. 706-756.
7. Mallik GB, Mirchandani JJ, Chitra S. Placenta in intrauterine growth retardation. J Obstet Gynaecol India .1979; 29: 805-10.
8. Cibilis LA. The placenta and newborn infant with hypertension conditions. Am J Obstet Gynaecol. 1974; 118:256-70.
9. Juan Rosai. Surgical Pathology.10th ed. New York. Elsevier. 2011.1649.
10. Kher AV, Zawar MP. Study of placental pathology in toxemia of pregnancy and its fetal implications. Indian J Pathol Microbiol. 1981; 24:245-51.
11. Bandana Das, Dutta D, Chakraborthy S, Nath P. Placental morphology in hypertensive disorders of pregnancy and its correlation with fetal outcome. J Obstet and Gynecol India. 1996; 46(1) :40-46.
12. Udainia A, Bhagwat SS, Mehta CD. Relation between placental surface area, infarction and foetal distress in pregnancy induced hypertension with its clinical relevance. J Anat Soc Ind. 2004; 53 : 27-30.
13. Narsimha A, Vasudeva DS. Spectrum of changes in placenta in toxaemia of pregnancy. IAPM. 2011; 54:15-20.
14. Fox H. General pathology of the placenta. In: Fox H, editor. Haines and Taylor Obstetrical and Gynecological Pathology. 4th ed. Edinburgh: Churchill Livingstone; 1995. 1480-2.
15. Goswami P, Lata H, Memon S, Khaskheli LB. Excessive Placental Calcification Observed in PIH Patients and its Relation to Fetal Outcome. JLUMHS. 2012;11(03):143-148.
16. Kurdukar MD, Deshpande NM, Shete SS, Zawar MP. Placenta in PIH. Indian J Pathol Microbiol. 2007 ; 50 (3):493-7.
17. Nobis P, Das U. Placental morphology in hypertensive pregnancy. J Obstet Gynecol .1990 ; 40:166-9.
18. Browne JC, Veall N. The maternal blood flow in normotensive and hypertensive women. J Obstet Gynaecol Br Emp. 1953 ; 60:141-7.
19. Sayeed M, Chakrawarti RN, Devi PK. A comparative study of placental villous changes in normal and abnormal pregnancies. J Obstet Gynaecol India .1976; 26 : 217-21.20.
20. Kalra VB, Aggarwal A, Sareen PM. Histopathological changes in placenta in toxemia of pregnancy. J Obstet Gynaecol India. 1985; 35: 86.
21. Maqueo M, Azuela JC, Manuel Dosal de la Vega. Placental pathology in eclampsia and pre-eclampsia. Obstet Gynaecol. 1964; 24: 350.
22. Kristina L, Raanan S, Rebecca B. Synctial knots as a Reflection of Placental Maturity : Reference values for 20 to 40 weeks gestational age.In: Pediatric and Developmental Pathology.2009; 28: 28-37.
23. AEP, Moll SJ, Jones CJ, Baker PN, Crocker IP. Formation of syncytial knots is increased by hyperoxia, hypoxia and reactive oxygen species. Placenta 28 2007(Suppl A):33-40.
24. Masodkar AR, Kalamkar LR, Patke PS. Histopathology of placenta and its correlation with fetal outcome. J Obstet Gynaecol India. 1985; 35:294-7.
25. Fox H. The incidence and significance of vasculosyncytial membranes in the human placenta. J Obstet. Gynaec Brit.C\rquote Wealth. 1967; 74:28.
26. Fox H, Basement membrane changes in the villi of human placenta. J Obstet Gynaecol Brit C\rquote Wealth. 1968 ; 75:302.
27. Sodhi S, Mohan H, Jaiswal TS, Mohan PS, Rathee S. Placental pathology in pre eclampsia- eclampsia syndrome. Indian J Pathol Microbiol. 1990;33:11-6.
28. Burstein R, Frankel S, Soule S.D et al. Ageing of the placenta: Autoimmune theory of senescence. Am J Obstet Gynaecol.1973; 116:271.
2. Jain K, Kavi V, Raghuveer C et al . Placental Pathology in PIH with or without IUGR. Indian J. Pathol. Microbiol.2007; 50 (3) : 533-537.
3. Emin M, Anna I. Bakardjiev, Susan J. The placenta : transcriptional, epigenetic, and physiological integration during development. J Clin Invest. 2010; 120(4) : 1016–25.
4. Udainia A, Jain ML. Morphological study of placenta in pregnancy induced hypertension with its clinical relevance, J Anat Soc. India. 2001; 50(1): 24-27.
5. Fernando Arias. In: Mosby. Practical guide to high-risk pregnancy and delivery. 2nd Edition. Harcourt Asia Private Ltd; 2000:184-185.
6. Cunningham F, Leveno K, Bloom S, Hanth J, Rouse D, Spong C. Pregnancy hypertension. In: Williams Obstetrics. 23rd ed. New York : McGraw Hill ; 2009. 706-756.
7. Mallik GB, Mirchandani JJ, Chitra S. Placenta in intrauterine growth retardation. J Obstet Gynaecol India .1979; 29: 805-10.
8. Cibilis LA. The placenta and newborn infant with hypertension conditions. Am J Obstet Gynaecol. 1974; 118:256-70.
9. Juan Rosai. Surgical Pathology.10th ed. New York. Elsevier. 2011.1649.
10. Kher AV, Zawar MP. Study of placental pathology in toxemia of pregnancy and its fetal implications. Indian J Pathol Microbiol. 1981; 24:245-51.
11. Bandana Das, Dutta D, Chakraborthy S, Nath P. Placental morphology in hypertensive disorders of pregnancy and its correlation with fetal outcome. J Obstet and Gynecol India. 1996; 46(1) :40-46.
12. Udainia A, Bhagwat SS, Mehta CD. Relation between placental surface area, infarction and foetal distress in pregnancy induced hypertension with its clinical relevance. J Anat Soc Ind. 2004; 53 : 27-30.
13. Narsimha A, Vasudeva DS. Spectrum of changes in placenta in toxaemia of pregnancy. IAPM. 2011; 54:15-20.
14. Fox H. General pathology of the placenta. In: Fox H, editor. Haines and Taylor Obstetrical and Gynecological Pathology. 4th ed. Edinburgh: Churchill Livingstone; 1995. 1480-2.
15. Goswami P, Lata H, Memon S, Khaskheli LB. Excessive Placental Calcification Observed in PIH Patients and its Relation to Fetal Outcome. JLUMHS. 2012;11(03):143-148.
16. Kurdukar MD, Deshpande NM, Shete SS, Zawar MP. Placenta in PIH. Indian J Pathol Microbiol. 2007 ; 50 (3):493-7.
17. Nobis P, Das U. Placental morphology in hypertensive pregnancy. J Obstet Gynecol .1990 ; 40:166-9.
18. Browne JC, Veall N. The maternal blood flow in normotensive and hypertensive women. J Obstet Gynaecol Br Emp. 1953 ; 60:141-7.
19. Sayeed M, Chakrawarti RN, Devi PK. A comparative study of placental villous changes in normal and abnormal pregnancies. J Obstet Gynaecol India .1976; 26 : 217-21.20.
20. Kalra VB, Aggarwal A, Sareen PM. Histopathological changes in placenta in toxemia of pregnancy. J Obstet Gynaecol India. 1985; 35: 86.
21. Maqueo M, Azuela JC, Manuel Dosal de la Vega. Placental pathology in eclampsia and pre-eclampsia. Obstet Gynaecol. 1964; 24: 350.
22. Kristina L, Raanan S, Rebecca B. Synctial knots as a Reflection of Placental Maturity : Reference values for 20 to 40 weeks gestational age.In: Pediatric and Developmental Pathology.2009; 28: 28-37.
23. AEP, Moll SJ, Jones CJ, Baker PN, Crocker IP. Formation of syncytial knots is increased by hyperoxia, hypoxia and reactive oxygen species. Placenta 28 2007(Suppl A):33-40.
24. Masodkar AR, Kalamkar LR, Patke PS. Histopathology of placenta and its correlation with fetal outcome. J Obstet Gynaecol India. 1985; 35:294-7.
25. Fox H. The incidence and significance of vasculosyncytial membranes in the human placenta. J Obstet. Gynaec Brit.C\rquote Wealth. 1967; 74:28.
26. Fox H, Basement membrane changes in the villi of human placenta. J Obstet Gynaecol Brit C\rquote Wealth. 1968 ; 75:302.
27. Sodhi S, Mohan H, Jaiswal TS, Mohan PS, Rathee S. Placental pathology in pre eclampsia- eclampsia syndrome. Indian J Pathol Microbiol. 1990;33:11-6.
28. Burstein R, Frankel S, Soule S.D et al. Ageing of the placenta: Autoimmune theory of senescence. Am J Obstet Gynaecol.1973; 116:271.
Published
2017-02-19
Issue
Section
Original Article
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access at http://opcit.eprints.org/oacitation-biblio.html).




