A hospital based study of Hb variant and beta thalassaemia mutational pattern characterization among the people of Northeast region of India
Keywords:
Haemoglobinopathies, thalassaemia, Hb Variants, HPLC, ARMS-PCR, Beta thalassaemia mutation.
Abstract
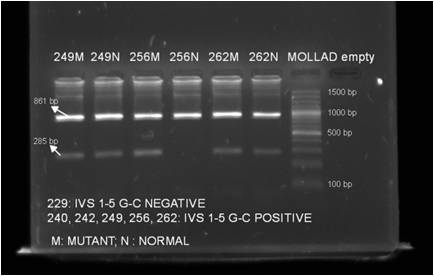
Background: Haemoglobinopathies and thalassaemia are the most common genetic disorders prevalent worldwide. In North East India, Hb E, β- thalassaemia, Hb S and Compound HbE-β thalassaemia are the most prevalent Hb variants. Aim:Detection of Hb variants are done by High Performance Liquid Chromatography (HPLC) based Haemoglobin testing system. The beta thalassaemia mutation is being analyzed here to get first hand information on the type of beta thalassaemia mutation prevailing among the population of Northeast region of India.Methods: The Hb variants were identified by HPLC based method and the beta thalassaemia mutations namely IVS 1-5 (G->C), IVS 1-1 (G->A), IVS 1-1 (G-T), Codon 8/9 and Codon 41/42 were characterized by ARMS-PCR.Results: Among the 460 cases referred for Hb variant diagnosis, 313 (68.04%) were positive for Haemoglobinopathies or thalassaemias and the rest 147 (31.96%) did not have any type of haemoglobinopathies or thalassaemia. Total 149 cases were having either beta thalassaemia major, beta thalassaemia minor or compound heterozygous with beta thalassaemia. The mutational patterns were identified, in 105 samples (70.469%) and in the rest 44 samples (29.53%) the mutational patterns remained uncharacterized. Among the 105 samples, 63.09% were positive for IVS 1-5 (G->C) mutation and 7.38% were positive with Codon 41/42 mutation.Conclusion: This preliminary information regarding the Hb variants occurrence and mutational pattern is important for establishing prenatal diagnosis programmes. The results showed that, Haemoglobinopathies and thalassaemia are common among the people of North east region of India and need counseling and awareness programme to reduce the risk of occurrence of this genetic disorder.References
1. Das R. Disorders of Haemoglobin Structure and Synthesis. In: Saxena R, Pati HR, Mahapatra M, editors. deGruchy’s Clinical Haematology in Medical Practice, 6thed. Wiley India Pvt. Ltd.; 2013. 120-145.
2. Krafft A, Breymann C. Haemoglobinopathy in Pregnancy: Diagnosis and Treatment. Current Medicinal Chemistry. 2004; 11 (21):2903-2909.
3. Fucharoen S, Winichagoon P. Haemoglobinopathies in Southeast Asia: molecular biology and clinical medicine. Haemoglobin. 1997; 21: 299-319.
4. Lukens JN. The abnormal hemoglobins: General Principles. In Lee GR, Foerster J, Lukens JN, Paraskevas F, Greer JP and Rodgera GM editors. Wintrobe’s Clinical Hematology, 10th ed.Maryland, USA: William & Wilkins publisher; 1999. 1329-1345.
5. Goldbloom RB. Screening for Haemoglobinopathies in Canada. In: Canadian Task Force on the Periodic Health Examination. Canadian Guide to Clinical Preventive Health Care. Ottawa: Health Canada.
6. Baruah MK, Saikia M, Baruah A. Pattern of hemoglobinopathies and thalassemias in upper Assam region of North Eastern India- High performance liquid chromatography studies in 9000 patients. Indian J PatholMicrobiol.2014;57:236-43.
7. Mohanty D, Colah RB, Gorakshakar AC, et.al. Prevalence of beta thalassaemia and other Haemoglobinopathies in six cities in India- a multi centre study. J. Community Genetic. 2013; 4: 33-42.
8. Ghosh N, Chakrabarti I, Chakraborty M, Goswami BK. A community based pilot study on prevalence of haemoglobinopathies among the antenatal women in a rural area of Darjeeling district, West Bengal. Int J Med Public Health. 2013; 3:107-10.
9. Rund D, Rachmilewitz E. Beta-thalassemia. New Eng. J. Med. 2005; 353(11): 1135-46.
10. Owen TM, Chan KD, Dietz L, Zehnder JL, Schrijver I. Comprehensive and Efficient HBB Mutation Analysis for Detection of Hemoglobinopathies in a Pan-Ethnic Population. Am J ClinPathol. 2010; 133:700-707.
11. Balgir RS. The Burden of haemoglobinopatheies in India and the challenges ahead. Current Science. 2010; 79 (11): 1536-1547.
12. Grow K, Vashist M, Abrol P, Sharma S, Yadav R. Beta thalassaemia in India- current status and the challenges ahead. International Journal of Pharmacy and Pharmaceutical Sciences. 2014; 6(4): 28-33.
13. Verma IC, Saxena R, Thomas E, Jain PK. Regional distribution of beta thalassaemia mutations in India. Human Genetics. 1997; 100 (1): 109-13.
14. Dastidar DG, Dutta RN, Gupta P, Old JM. Detection of beta thalassaemia mutation in eastern Indian population by polymerase chain reaction. Indian J Med Res. 1994; 100: 111-114.
15. Satpute SB, Bankar MP, Momin AA. The prevalence of β-thalassaemia mutations in south western Maharashtra. Indian Journal of Clinical Biochemistry. 2012; 27(4); 389-393.
16. Instruction Manual.pocH-100i, SYSMEX Corporation, Kobe, Japan, Asia Pacific Edition B.
17. Instruction Manual. D-10 Dual Program, Bio-Rad Laboratories, United States.
18. Ithanet Electronic Infrastructure for Thalassaemia Research Network. Protocol for Amplification Refractory Mutation System (ARMS). Available from http://portal.ithanet.eu.
19. Varawalla NY, Old JM, Sarkar R, Venkatesan R, Weatherall DJ. The spectrum of beta thalassaemia mutations on the Indian subcontinent- the basis for prenatal diagnosis. Br.J. Hematol. 1991; 78:242-247.
20. Panigrahi I, Marwaha RK. Mutational spectrum of thalassaemias in India. Indian Journal of Human Genetics. 2007; 13(1): 36-37.
21. Sinha S, Black ML, Agarwal S, Colah R. et. al. Profiling beta thalassaemia mutations in India at state and regional levels- implications for genetic education, screening and counseling programmes. The HUGO Journal.2009; 3:51-62.
22. Vaz FEE, Mahadik CBT, Banerjee MK, Gangal SG. Distribution of beta thalassaemia mutations in Indian population referred to a diagnostic center. Hemoglobin. 2000, 24(3): 184-194.
2. Krafft A, Breymann C. Haemoglobinopathy in Pregnancy: Diagnosis and Treatment. Current Medicinal Chemistry. 2004; 11 (21):2903-2909.
3. Fucharoen S, Winichagoon P. Haemoglobinopathies in Southeast Asia: molecular biology and clinical medicine. Haemoglobin. 1997; 21: 299-319.
4. Lukens JN. The abnormal hemoglobins: General Principles. In Lee GR, Foerster J, Lukens JN, Paraskevas F, Greer JP and Rodgera GM editors. Wintrobe’s Clinical Hematology, 10th ed.Maryland, USA: William & Wilkins publisher; 1999. 1329-1345.
5. Goldbloom RB. Screening for Haemoglobinopathies in Canada. In: Canadian Task Force on the Periodic Health Examination. Canadian Guide to Clinical Preventive Health Care. Ottawa: Health Canada.
6. Baruah MK, Saikia M, Baruah A. Pattern of hemoglobinopathies and thalassemias in upper Assam region of North Eastern India- High performance liquid chromatography studies in 9000 patients. Indian J PatholMicrobiol.2014;57:236-43.
7. Mohanty D, Colah RB, Gorakshakar AC, et.al. Prevalence of beta thalassaemia and other Haemoglobinopathies in six cities in India- a multi centre study. J. Community Genetic. 2013; 4: 33-42.
8. Ghosh N, Chakrabarti I, Chakraborty M, Goswami BK. A community based pilot study on prevalence of haemoglobinopathies among the antenatal women in a rural area of Darjeeling district, West Bengal. Int J Med Public Health. 2013; 3:107-10.
9. Rund D, Rachmilewitz E. Beta-thalassemia. New Eng. J. Med. 2005; 353(11): 1135-46.
10. Owen TM, Chan KD, Dietz L, Zehnder JL, Schrijver I. Comprehensive and Efficient HBB Mutation Analysis for Detection of Hemoglobinopathies in a Pan-Ethnic Population. Am J ClinPathol. 2010; 133:700-707.
11. Balgir RS. The Burden of haemoglobinopatheies in India and the challenges ahead. Current Science. 2010; 79 (11): 1536-1547.
12. Grow K, Vashist M, Abrol P, Sharma S, Yadav R. Beta thalassaemia in India- current status and the challenges ahead. International Journal of Pharmacy and Pharmaceutical Sciences. 2014; 6(4): 28-33.
13. Verma IC, Saxena R, Thomas E, Jain PK. Regional distribution of beta thalassaemia mutations in India. Human Genetics. 1997; 100 (1): 109-13.
14. Dastidar DG, Dutta RN, Gupta P, Old JM. Detection of beta thalassaemia mutation in eastern Indian population by polymerase chain reaction. Indian J Med Res. 1994; 100: 111-114.
15. Satpute SB, Bankar MP, Momin AA. The prevalence of β-thalassaemia mutations in south western Maharashtra. Indian Journal of Clinical Biochemistry. 2012; 27(4); 389-393.
16. Instruction Manual.pocH-100i, SYSMEX Corporation, Kobe, Japan, Asia Pacific Edition B.
17. Instruction Manual. D-10 Dual Program, Bio-Rad Laboratories, United States.
18. Ithanet Electronic Infrastructure for Thalassaemia Research Network. Protocol for Amplification Refractory Mutation System (ARMS). Available from http://portal.ithanet.eu.
19. Varawalla NY, Old JM, Sarkar R, Venkatesan R, Weatherall DJ. The spectrum of beta thalassaemia mutations on the Indian subcontinent- the basis for prenatal diagnosis. Br.J. Hematol. 1991; 78:242-247.
20. Panigrahi I, Marwaha RK. Mutational spectrum of thalassaemias in India. Indian Journal of Human Genetics. 2007; 13(1): 36-37.
21. Sinha S, Black ML, Agarwal S, Colah R. et. al. Profiling beta thalassaemia mutations in India at state and regional levels- implications for genetic education, screening and counseling programmes. The HUGO Journal.2009; 3:51-62.
22. Vaz FEE, Mahadik CBT, Banerjee MK, Gangal SG. Distribution of beta thalassaemia mutations in Indian population referred to a diagnostic center. Hemoglobin. 2000, 24(3): 184-194.
Published
2016-08-09
Issue
Section
Original Article
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access at http://opcit.eprints.org/oacitation-biblio.html).